Lessons from the field: Canadian doctor offers a global perspective on the COVID-19 pandemic

Having worked on the front lines of both the SARS and Ebola epidemics and having spent much of her career focused on infectious diseases in the developing world, Dr. Adrienne Chan has seen a good deal that informs her thoughts and actions surrounding the COVID-19 pandemic.

Dr. Adrienne Chan at Zomba Central Hospital in southern Malawi - Credit: Ian Brown Photography
But the physician at Sunnybrook Health Sciences Centre in Toronto says it was a visit to a Zimbabwe hospital in 2005 that stays with her the most.
As a medical student, Chan had watched the development and roll-out of life-saving antiretroviral therapy (ART) medicines for HIV, which by the mid 1990s had all but brought an end to deaths from the disease in Canada. Yet a decade later, while walking through that hospital in southern Africa, “I witnessed wards full of adults and children dying of opportunistic infections that many physicians who trained in my generation in Canada had rarely seen.”
It was an eye-opening experience, to say the least.
“To be confronted so viscerally with the injustices of that disparity in access to treatment changed me as a physician and as a person,” recalls Chan. She feels that “the delay in the public roll-out of ART in low-resource settings is one of the greatest medical injustices of our time.”
Chan returned home to Canada “with the goal of contributing in a small way to the roll-out of ART in southern Africa, and to try to get ART to as many HIV patients as quickly as possible.”

Dr. Adrienne Chan with the team at the Tisungane Clinic - Credit: Ian Brown Photography
That’s what she did for 13 years alongside colleagues in Malawi, working for . She served there from 2007 to 2010 as the organization’s HIV clinic coordinator and country program medical coordinator, then travelled frequently to Malawi as a medical advisor for Dignitas from 2010 to 2019.
Chan’s other experiences with epidemics included working as a third-year resident during the 2003 SARS outbreak in Toronto, where she saw “how important it is to have leadership presence at the front lines.” She also served as a clinical consultant for the World Health Organization’s Department of Pandemic and Epidemic Diseases, conducting training with its Ebola response team in Sierra Leone from December 2014 to February 2015.
The infectious diseases physician learned many lessons from that experience, “but I think one of the most important things is that you can’t manage outbreaks from a computer,” Chan says. “It requires on-site management, working hand-in-hand with front-line service providers, especially when it comes to novel and high-consequence pathogens.”
Early and ongoing community engagement by health professionals, especially understanding the populations disproportionately affected by an outbreak, is also “key in crafting an effective public-health response, and something that I think we aren’t always great at doing,” she remarks.

Dr. Adrienne Chan, a physician at Sunnybrook Health Sciences Centre in Toronto - Credit: Sunnybrook Health Sciences Centre
After Sunnybrook treated Canada’s in January 2020 and began supporting area long-term care homes devastated by the virus, Chan became associate medical director of infection prevention and control at the hospital, putting her experience in outbreak management to work. When it recently marked the one-year anniversary of that first case, the hospital had managed more than 4,000 patients with COVID‑19.
Chan says that “one of the happiest points in a challenging year” was knowing that all of the care homes that Sunnybrook deals with had been offered vaccines, with high resident uptake. All workers there had also been offered the vaccine.
Today Chan serves on the board of directors of , a health and social justice organization whose mission lies in the idea of solidarity with vulnerable populations. She says it has translated lessons learned from its work in HIV, tuberculosis and Ebola in low-resource settings into building an effective COVID-19 contact-tracing infrastructure in different parts of North America.
Contact-tracing and community engagement are the “cornerstones of any good public health response,” comments Chan. “Because communicable disease is often inextricably linked to stigma and marginalization, community engagement has to occur for response efforts to be successful.”
She comments that the “rapidity with which science has been able to develop multiple COVID vaccines is truly a remarkable achievement.” While Canadians question the pace of immunizations, “I think we have forgotten that for billions of people globally, the vaccine will not be available until 2022 or even later,” says Chan. She thinks it could take up to four years to manufacture enough doses to vaccinate the global population.
“We are far more interconnected now than we were 25 years ago, and it’s critical that we don’t repeat the same mistake of leaving poor countries behind yet again,” she cautions. Indeed, lessons learned from the global HIV response should be quickly adopted for COVID-19 immunization, Chan says.
This means vaccines should be affordable and equitably distributed, prioritizing those most at risk including the elderly, chronically ill, health providers and communities disproportionately affected by COVID-19, following “data-driven approaches.” And community engagement should be a critical part of the planning and implementation of the vaccine roll-out.
“The lessons of the past have shown us that fear, denial, complacency, stigma and inequity in particular have deep human costs that affect everyone,” says Chan, who points out that lower-resource countries are not able to bulk-purchase vaccine like Canada can.
“I think sometimes people forget that until the virus is controlled everywhere, every country—including Canada—is at risk of ongoing outbreak.” Chan warns that without support for these poorer populations, “it will take longer for the pandemic to end for all of us.”
Canada supports equitable vaccine access worldwide
Canada is committed to a robust, comprehensive, global effort to stop the COVID-19 pandemic and address its devastating health, social and economic impacts on people in developing countries.
Since February 2020, the Government of Canada has announced that it has committed to the global response to COVID-19. This includes more than $865 million in financing for the , a platform to mobilize and coordinate the global effort needed for the equitable development, production and distribution of safe, affordable and effective COVID-19 tests, treatments and vaccines.
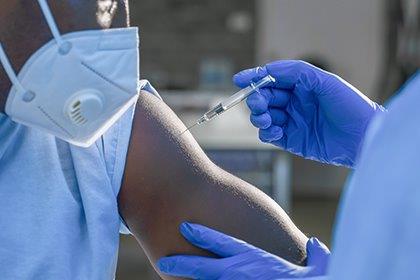
Equitable access to an affordable COVID-19 vaccine by all countries is an essential part of this global response. To achieve this goal, a mechanism to pool the procurement of COVID-19 vaccines across a large number of countries has been created by Gavi, the Vaccine Alliance, as well as the Coalition for Epidemic Preparedness Innovations and the World Health Organization.
Called the COVAX Facility, the initiative supports collective efforts to foster fair, equitable and timely access to vaccines for 190 participating economies around the world, representing nearly 90% of the global population. Its innovative financing instrument enables higher-income countries to finance their own purchase of vaccine doses for domestic use. Meanwhile, 92 low- and middle-income countries can acquire vaccines to immunize up to 20% of their population with the support of official development assistance financing, and they can cost-share for additional doses beyond those donor-subsidized ones.
Canada is among the , through the COVAX Advance Market Commitment to support low- and middle-income countries. Supporting countries in their fight against COVID-19 and other infectious diseases is an investment to protect Canada and Canadians.
- Date modified: